Fulfilling your dream of having a family is not always easy. But it can be an exciting and hopeful time. Your biggest peace of mind should be to know that the physicians you choose for your care are board certified and qualified specialists in Reproductive Endocrinology and Infertility. You can feel confident that, without a doubt, The Reproductive Medicine Group consists of board certified Reproductive Endocrinologists, which are also known as fertility doctors. Our group of physicians is the largest fertility clinic in the Tampa Bay, with five physicians locally that are board certified in Obstetrics and Gynecology, as well board certified in Reproductive Endocrinology and Infertility.
Our fertility specialists trained at medical facilities in the United States including Harvard, UCLA and Johns Hopkins. Our physicians have consistently been selected by their peers as “Best Doctors in America – Fertility” by US News and World Reports, Tampa Magazine’s Top Docs – Fertility, and Tampa Bay Metro’s “Top Doctors – Fertility”. We participate in the most current research programs to bring new treatment technologies to our practice, and to our patients. The diplomas on our walls may show our education and experience, but it’s our patients who give us the biggest rewards.
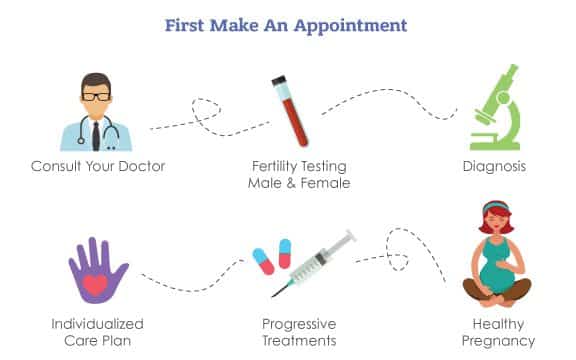
A consultation with a fertility specialist is a first step to understand infertility.
From the moment you begin your experience with The Reproductive Medicine Group, you should feel comfortable openly and honestly communicating with everyone in any of our offices. No matter how simple or complex your medical treatment, we pay particular attention to make sure you are treated with personal care every step along the way. Never hesitate to ask questions or take more time with any of our team members at the front desk or in the operating room.
Before undergoing any tests or treatment, you will:
- Review your reproductive and medical history
- Evaluate you for signs of infertility
- Perform a medical examination
- Discuss fertility treatment options.
At The Reproductive Medicine Group, you and your partner are a vital part of the treatment equation; therefore we suggest the two of you attend this initial consultation. It’s also possible that you may need additional diagnostic testing before your physician can make a final recommendation.
If no further tests are requested, your physician will create an optimal treatment plan specific to your fertility issues and comfort level. Once you begin treatment, you may set up additional meetings with your physician to discuss any issues or concerns about your progress or an upcoming procedure. Even when you aren’t seeing your doctor, please know your physician will be monitoring your fertility treatment. Our nurses will be in constant contact with your physician at all times, following your progress.
Now let’s review some basic fertility information, so you can better
understand your fertility health and your infertility treatment options.
“When it comes to your fertility, every day counts.”
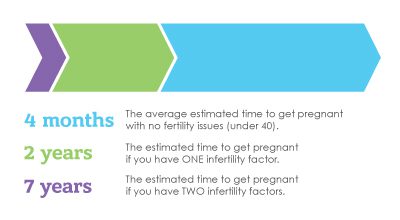
It is often possible for you to have some control over your fertility. How? By taking charge of your fertility health whether you want to get pregnant now or later. Our patient’s most common regret is that they didn’t seek help from us sooner. The earlier treatment is started, the better the chances of success. There is also a better possibility of using less invasive fertility procedures.
Many of our patients realize there is a fertility problem when they start “trying to conceive”. Ironically, most of our education around conception comes from NOT trying to get pregnant. So when the time comes for you to start your family, you may think that pregnancy will quickly occur. Getting pregnant is natural, right?
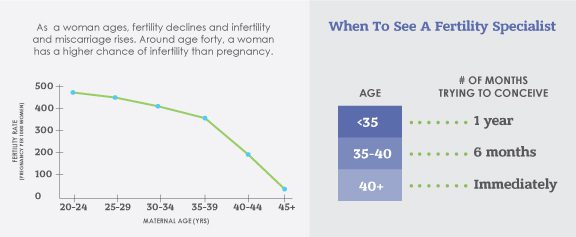
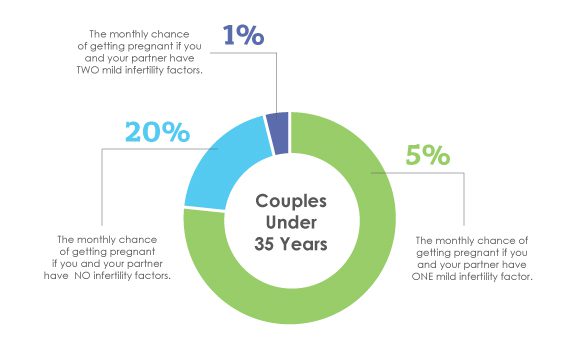
For some, that is true. Most couples will experience pregnancy in the first year of trying to conceive. However, as many as 20 percent of men and women will discover they struggle with their fertility problems.
What is infertility?
Simply stated, infertility is not getting pregnant after 6 to 12 months of not using any form of prevention or birth control. You may call it “trouble getting pregnant”. It can also be the inability to sustain a pregnancy, resulting in recurrent or repeat miscarriage. Sometimes, there are early signs of infertility that suggest that difficulty with conceiving may occur.
Successful pregnancy requires several factors from both male and female partner. These include:
- The man and woman’s bodies creating sperm and eggs
- The sperm and egg successfully meeting and resulting into a fertilized embryo
- The embryo attaching to the uterine wall and developing for 37-40 weeks
Understanding the Impact of 1-2 Infertility Factors:
Issues identified with EITHER or both the man or woman during fertility testing can cause or contribute to infertility problems. This is also true for couples who are having trouble sustaining a pregnancy. (with 2 or more miscarriages), or what’s called recurrent miscarriage. What’s important is that couples seek early intervention, or if possible, prevention. Diagnosed, most male or female problems can be treated by a fertility doctor who is a specialist in testing and treatment. Reproductive Endocrinologists are surgeons and experts in helping women get pregnant and sustain pregnancies. They are also experts in hormone disorders, and are specialists in IVF (In Vitro fertilization), among other fertility treatments.
Here’s a look at both male and female reproduction. It’s important that both partners be tested to identify potential infertility. And yes – infertility CAN be treated.
Reasons for infertility:
- Male infertility
- Female infertility
- Combination of male/female infertility
- Unexplained infertility
- Recurrent Pregnancy Loss
Here’s a look at both male and female reproduction. It’s important that both partners be tested to identify potential infertility. And yes – Infertility CAN be treated.
Types of infertility:
- Male factor infertility
- Female factor infertility
- Combination (male/female) infertility
- Unexplained infertility
Female Infertility: Anatomy
It may have been a while since you had a lesson in a woman’s reproductive health. So, let’s review some of the basic details of a woman’s role in conception and how pregnancy occurs.
One major part of a woman’s fertility is the egg, also known as an oocyte, ovum, or gamete. A female is born with a pre-determined number of eggs – usually around 1-2 million in total. These eggs are formed while she is in her mother’s womb, before a woman is even born! By the time a woman is in her early to mid-50’s, a few hundred eggs or less remain in her ovaries. This is one reason why age is one of the most important factors in a woman’s fertility. Age affects both egg quantity and egg quality. As a woman ages, so do her eggs. Ovarian reserve is a term used to describe the status of a woman’s quantity and quality of eggs remaining in the ovaries.
A female’s reproductive organs consist of the vagina, cervix, uterus, fallopian tubes, and the ovaries. The vagina is the tube that connects the external opening to the cervix. The cervix is the tissue that serves as the entry into the uterus. Both the vagina and the uterus have muscular walls, but the uterus has a thick lining. This lining will allow an embryo to implant and a baby to grow. Each month blood and tissue build inside the uterus. If a woman’s egg is not fertilized, she will not become pregnant and will shed the lining as her monthly period.
On either side of the uterus, two fallopian tubes extend from the uterus toward each ovary. The ovaries store, mature, and release eggs into the fallopian tubes during ovulation. The fallopian tubes are the location where sperm and egg meet and fertilize. The tubes are narrow at the top near their connection to the uterus and wider toward the ends near the ovaries. The end of the tube is called the fimbriae. The fimbriae are delicate structures that are responsible for picking up the egg from the ovary. Infertility can occur if the fimbriae are damaged from:
- an infection such as gonorrhea or chlamydia
- scar tissue within or around the tubes due to prior surgery
- endometriosis
- tubal pregnancy
During each monthly menstrual cycle, an egg is released from one of the ovaries and travels through the fallopian tubes down to the uterus.
Ovaries produce the female hormones estrogen and progesterone. Not only do these hormones control the menstrual cycle, they also play a large role in getting pregnant and sustaining pregnancy. If hormone levels are too high or low, it can result in miscarriage.
The pituitary is a gland located in the brain. The pituitary also plays a role by releasing follicle stimulating hormone (FSH) and luteinizing hormone (LH) in order to regulate estrogen and progesterone. This allows for ovulation.
Female Infertility – Factors & Diagnosis
Female infertility causes include:
- inadequate egg quality or quantity (low ovarian reserve)
- problems with hormones levels affecting ovulation
- pelvic scarring or inflammation
- endometriosis
- fallopian tube damage or blockage
- uterine polyps and fibroids.
Another fertility issue that women can face is recurrent pregnancy loss, which is when a woman has had 2 or more miscarriages.
Some diagnosis related to female infertility factor are:
- Ovulation Disorders
- PCOS (Polycystic Ovarian Syndrome)
- Endometriosis
- Premature Ovarian Failure (POF)
- Uterine Fibroids and Polyps
- Recurrent Pregnancy Loss
- Advanced Maternal Age
- Tubal Abnormalities or Prior Tubal Ligation
Ovulation Disorders
Any disruption in the monthly process of ovulation can result in female infertility. Often, women with ovulation problems will experience irregularities in their menstrual cycles. Testing can be done to determine if a woman is ovulating. Testing for polycystic ovary syndrome (PCOS), thyroid, and/or prolactin disorders can be done. Reproductive Endocrinologists specialize in diagnosing and treating PCOS as well as other hormone disorders that affect fertility.
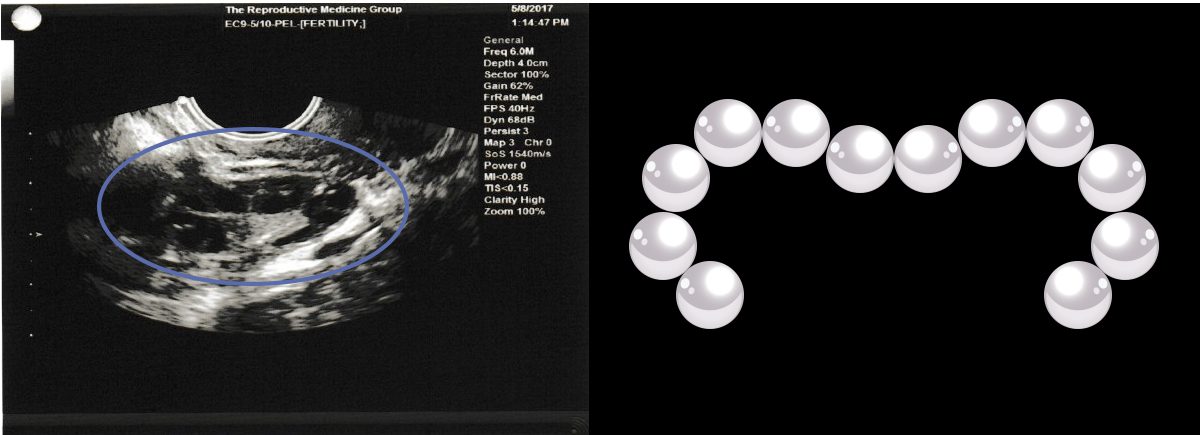
Polycystic Ovarian Syndrome (PCOS)
PCOS is a common cause of not ovulating regularly, irregular periods, and female factor infertility. It is also called Polycystic Ovaries (PCO) or Polycystic Ovarian Disease (PCOD). Women who have PCOS experiencing infertility do not mature and release an egg each month. They also have ovaries which house many small cysts, which can be as big as a marble or as small as a coarse grain of salt.
Treatment for PCOS with infertility may include medications to stimulate the ovaries.
Polycystic Ovarian Syndrome – PCOS by Sandy Goodman, M.D.
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder occurring in women 10 to 45 years old. Approximately 5–10% of women (3.5 to 5 million women) in the United States are affected. Females with PCOS often experience irregular, heavy or absent menstral bleeding, facial, abdominal or lower back hair growth (hirsutism), hair loss from the top of the head, acne, obesity and infertility. Irregular menstral bleeding can manifest by menstral cycles that are longer than 35 days apart or by bleeding episodes shorter than 21 days apart. Both patterns suggest a disruption in the ovulation (egg development and release) process.
Etiology
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder occurring in women 10 to 45 years old. Approximately 5–10% of women (3.5 to 5 million women) in the United States are affected. Females with PCOS often experience irregular, heavy or absent menstrual bleeding (periods), facial, abdominal or lower back hair growth (hirsutism), hair loss from the top of the head, acne, obesity and infertility in women. Irregular periods (menstrual bleeding) can manifest by menstrual cycles that are longer than 35 days apart or by bleeding episodes shorter than 21 days apart. Both patterns suggest a disruption in the ovulation (egg development and release) process.
The cause of PCOS has not been completely determined although genetics likely play a role. A family history of diabetes, obesity, irregular menses or hirsutism is common. The majority of patients have a higher than normal amount of luteinizing hormone (LH) in relationship to follicle stimulating hormone (FSH) produced by the pituitary gland (a small gland located at the base of the brain). Additionally, numerous studies have linked hyperinsulinemia (high blood levels of the hormone insulin) with PCOS. Elevation in the amount of LH produced decreases the chances that an egg will develop and be released. The ovary continues to produce estrogen as well as an excess male hormone including testosterone. Continual estrogen production stimulates growth of the uterine (endometrial) lining. In females who ovulate regularly and do not have PCOS, estrogen is counter balanced by progesterone which is released after ovulation. Progesterone stabilizes the endometrial lining.
In PCOS women, without ovulation, progesterone is not produced. The resultant unopposed estrogen causes the development of a thickened and irregular endometrial lining that can result in abnormal bleeding, hemorrhage, or pre-cancerous changes which can eventually development into uterine cancer. Excessive production of male hormones further disrupts the menstrual cycle and causes acne as well as male pattern hair growth in areas including the face, chest, abdomen and lower back with hair loss in the front and top of the head. Additionally, up to 80% of women with PCOS have some degree of insulin resistance which results in the release of higher amounts on insulin into the blood than normal. Insulin stimulates ovarian as well as adrenal androgen secretion, further worsening hair abnormalities and acne. Excessive levels of androgens and insulin can affect metabolism and weight. Ultimately, insulin resistance can develop into actual diabetes. Women with PCOS often experience problems with weight control, frequently observing that they gain weight easily but experience significant difficulty losing weight.
Unfortunately, obesity has significant adverse effects on PCOS by worsening insulin resistance and glucose intolerance and increasing the amount of active male hormone. Numerous studies have demonstrated that even a 10% weight loss can have a significant, positive effect on the PCOS metabolic and hormone profile including improvement in insulin resistance, decline in male hormone levels and improvement in menstrual cycle regulation. Women with untreated PCOS are at increased risk for developing anemia, (low red blood cell count), endometrial hyperplasia/cancer, hypertension (high blood pressure) diabetes, lipid (cholesterol) abnormalities and cardiovascular (heart) disease. PCOS is a common cause of infertility and is also associated with pregnancy complications. First trimester (weeks 4 to 11) pregnancy loss rates have been noted to be as high as 30-40% for women with PCOS, in comparison to the 10-15% rate reported in the general population. Additionally, PCOS women are at increased risk for developing diabetes and hypertension during their pregnancy.
Diagnosis
Both the symptoms as well as the long-term health consequences of PCOS can be altered through a combination of lifestyle changes and medical management. All preteens, teenagers and woman with irregular menses in combination with either abnormal hair growth or acne should see their physician and request an evaluation for PCOS. Children may present as early as age 10 with hair growth or the disorder may not manifest until the 20’s or 30’s, often in association with weight gain. A physical exam should include assessment of height, weight with BMI (body mass index) calculation and blood pressure. Signs of excess hair, male pattern baldness, obesity and acanthosis nigricans (darkening of the skin behind the neck, under the arms, and on the inner thighs which indicates insulin resistance) may be visualized. Appropriate laboratory testing includes measurement of fasting glucose (blood sugar), insulin, FSH, LH, DHEAS, total testosterone, TSH, prolactin and lipid profile.
Treatment
Therapy for PCOS is determined by your goals in terms of desire for pregnancy or treatment of abnormal hair growth, acne, or obesity. Educating yourself about your health and actively participating in your care is essential for getting your PCOS under control. Regulation of the menstrual cycle is essential in avoiding long-term complications of heavy or prolonged uterine bleeding and endometrial hyperplasia/cancer. The cornerstone of therapy involves lifestyle changes incorporating dietary modifications and exercise. As noted, weight reduction of even 10% has been demonstrated to improve insulin resistance, reduce blood levels of male hormones, and improve lipid abnormalities. A high fiber, reduced carbohydrate diet has been beneficial to many PCOS women in achieving weight loss. Counseling with a nutritionist who has an interest in treating PCOS is recommended. Exercise has been demonstrated to improve insulin sensitivity as well as weight loss. After consultation with your physician, begin slowly but unless contraindicated, your goal should be cardiovascular aerobic exercise in which your heart rate is accelerated to between 120-140 beats per minute for 45 to 60 minutes daily. Unfortunately there is no magic pill currently available to cure PCOS but you can do your part to gain control through diet and daily exercise.
Insulin sensitizing agents have become an increasingly common element in the treatment regimen of PCOS. Metformin (glucophage) has been used to treat diabetes mellitus for more than 40 years and is currently the most widely used sugar lowering agent for women with PCOS. Metformin indirectly improves insulin resistance by decreasing the production of glucose (sugar) by the liver. In comparison with diet alone, metformin added to a low calorie, reduced carbohydrate diet has been demonstrated to result in greater reduction in body weight, abdominal fat, hirsutism, insulin resistance and androgen levels. Gastrointestinal side effects including bloating, nausea and diarrhea are the most frequent cause of drug discontinuation. Starting at a low dose with slow increases over time will minimize these side effects. Also, foods/drinks with high carbohydrate or simple sugar content worsen GI side effects. Evaluate your diet before giving up on the metformin/glucophage therapy. Some women tolerate the extended release formula better so ask your physician about that option if you cannot tolerate the regular formula. You should not take metformin if you have kidney, liver or severe heart disease. In addition, the medication should be temporarily discontinued before surgery, procedures requiring intravenous iodinated contrast media (such as hysterosalpingogram, IVP or CAT scan) and during a severe febrile (high fever) or dehydrating illness. The combination of weight loss and use of metformin may allow women who are not ovulating, but desire pregnancy,
to become ovulatory and conceive. Specific medications are available to stimulate ovulation for PCOS women who wish to conceive, including clomiphene citrate, letrozole (both taken orally) and gonadotropins (FSH or FSH/LH hormones) that are given by injections under the skin surface. Surgical treatment of PCOS by a method known as ovarian diathermy or drilling has been described in the medical literature. The procedure involves the use of a cautery needle to puncture the ovarian capsule during laparoscopy with the goal of reducing the amount of ovarian androgen producing tissue in order to improve the frequency of ovulation.
Birth control pills (OCP’s) have been the mainstay of treatment for girls and women with PCOS who are not pursuing fertility. OCP’s increase the release of sex hormone binding globulin which binds up the free/active male hormone, thereby lowering the testosterone level, decrease LH release which also decreases testosterone production and regulates the menstrual cycle. Although OCP’s have a role in the treatment of hirsutism, more than 60% of hirsute patients do not find OCP’s alone to be sufficiently effective in treating existing hair growth. In addition to androgen (male hormone) suppression from OCP’s, androgen blockers can be added to the treatment regimen for women struggling with hirsutism that does not adequately respond to OCPs. The principle medication used for this purpose in the United States is aldactone/spironolactone. Antiandrogenic medications are potential teratogens (are harmful to the unborn fetus/baby) and should be used in combination with reliable contraceptives, optimally with OCP’s and are not appropriate for use by women who are sexually active without the use of reliable contraception or who are desiring pregnancy.
Mechanical reduction of unwanted hair by tweezing, shaving, depilatories, electrolysis or laser hair removal are effective. Eflornithine hydrochloride (Vaniqua) has been available for use on facial hair. Vaniqua is applied to the skin and works by inhibiting an enzyme that effects hair growth and reverses the terminalization of the hairs being produced, making the facial hair lighter and less course. Skin irritation, cost and need for daily application are the most common reasons for a high discontinuation rate. Other than laser therapy, all mechanical methods are temporary and are best used in conjunction with androgen lowering medications. Laser hair removal is the most effective method but even with that treatment, control of the hormones with medication is important to allow the technique to be maximally effective.
PCOS remains a difficult and frustrating disorder with variable presenting signs and symptoms. Diagnosis is essential to allow for appropriate education and intervention. Menstrual irregularities, hirsutism and fertility issues should be addressed. Long-term health disorders including diabetes mellitus, endometrial cancer, hyperlipidemia and cardiovascular disease may be mitigated or avoided by lifestyle modifications in combination with appropriate medications.
Resources:
American College of Obstetricians and Gynecologists (ACOG) www.acog.org
American Society for Reproductive Medicine (ASRM) www.asrm.org
American Association of Clinical Endocrinology (AACE) www.aace.org
Polycystic Ovarian Syndrome Society (PCOS) www.pcosupport.org
This brochure has been written by Sandy B. Goodman, M.D. and is the sole property of The Reproductive Medicine Group, Tampa, FL.
Endometriosis
Endometriosis is a condition in which cells that are similar to the lining of the uterus (endometrial lining) grow outside of the uterus. Endometriosis can cause pain and infertility issues. Scar tissue, also called pelvic adhesions, can cause infertility. Scar tissue can be created by previous infection, previous surgery, or endometriosis. If the fallopian tubes are blocked or full of scar tissue, this can prevent the egg from traveling through the fallopian tubes down into the uterus. In some cases, this can lead to an ectopic or “tubal pregnancy”, where the embryo implants outside the uterus and in the fallopian tube.
Treatments for endometriosis may include:
- Laparoscopy (surgical removal of the endometriosis)
- Hormonal treatments that inhibit growth of endometriosis
- In-vitro fertilization (IVF)

Premature Ovarian Failure (POF)
Sometimes, women under the age of 40 will experience a sudden drop in ovarian function that is like an early menopause. This is referred to as premature ovarian failure or premature ovarian insufficiency. Sometimes, the cause is unknown, but other times it may relate to autoimmune, genetic, or environmental factors such as exposure to chemotherapy.
Treatments for POF may include use of an egg from a donor who is young and has a large number of healthy eggs.
Uterine Fibroids and Polyps
Uterine fibroids are benign muscle tumors within the uterus. Fibroids begin within the muscle wall of the uterus but can grow into the uterine cavity as well. A uterine polyp is an overgrowth of tissue, like a skin tag within the uterus. Both may potentially interfere with implantation of an embryo into the uterus lining.
Treatment for fibroids or polyps often includes surgical removal.
Advanced Maternal Age (Over 35 years old)
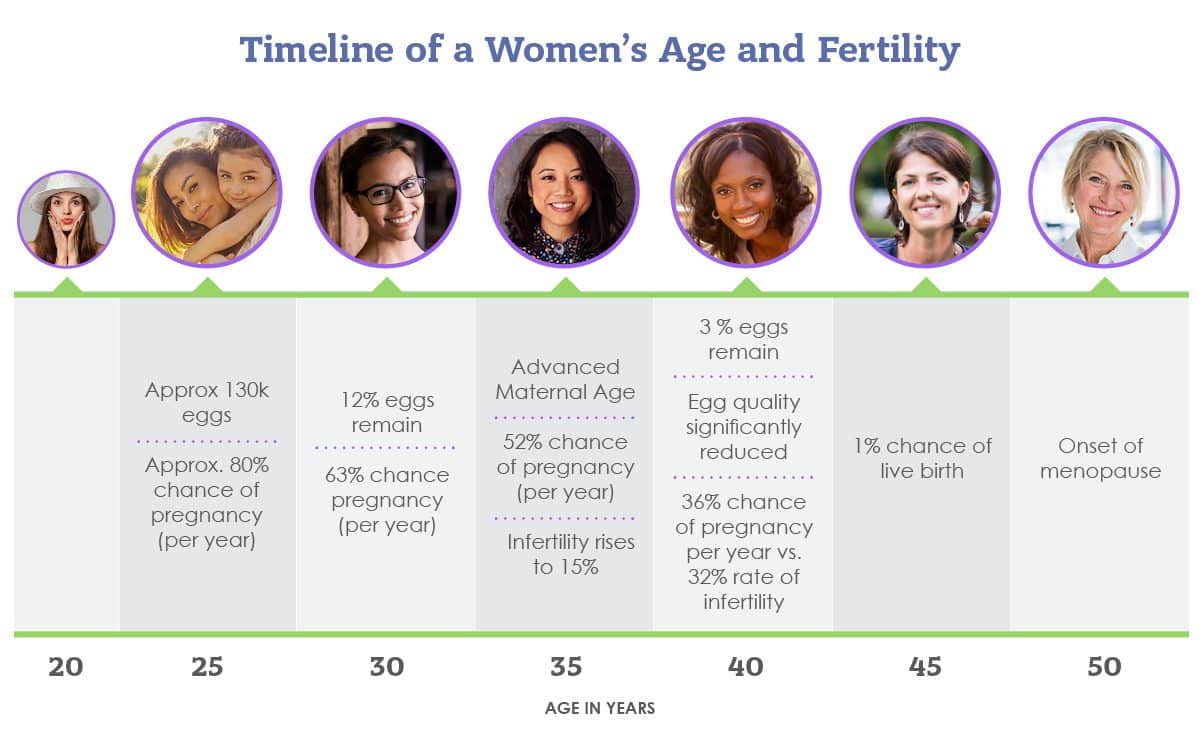
As women age, their egg quantity and egg quality decreases. If a woman chooses to delay child bearing because of financial, career, social or any other reasons, one option to preserve fertility is egg (or oocyte) cryopreservation.
Ovarian reserve is the ability of a woman’s remaining eggs in her ovaries at a given age, to produce a viable pregnancy. Typically all fertility patients, regardless of age, are given ovarian reserve testing to determine their fertility.
Decrease in ovarian reserve due to age, usually starts as a woman enters her mid-thirties. There is a significant decrease in female fertility beginning at age 33. At first, the decline is gradual, but becomes more rapid and substantial closer to age 40. Usually the older the maternal age, the more difficult it becomes to conceive.
Treatments may include In Vitro fertilization (IVF) and use of a donated egg from a young, healthy egg donor may be recommended.
Recurrent Pregnancy Loss
If you have experienced two or more miscarriages, you may need the help of a Reproductive Endocrinologist to:
- Identify causes of miscarriage
- Recommend treatment to increase the chances of sustaining pregnancy and delivering a healthy baby
Recurrent pregnancy loss, or recurrent miscarriage, is defined by the American Society for Reproductive Medicine (ASRM) as two or more pregnancy losses (miscarriages). A pregnancy loss is a pregnancy which involuntarily ended prior to 20 weeks. The pregnancy may have been confirmed by a pregnancy test, been visually identified on an ultrasound, or pregnancy tissue was identified after the pregnancy was lost.
Why did I miscarry my pregnancy?
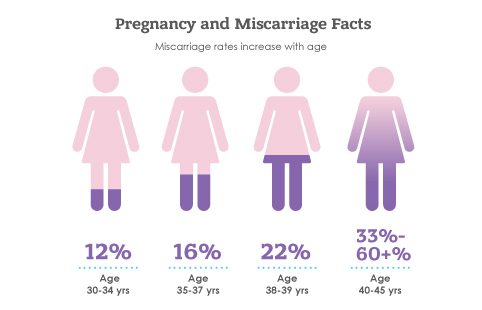
Most pregnancy losses are related to chromosomal or genetic abnormalities that are random, events. Chromosomal abnormalities may be caused by problems with the sperm, the egg, or with the early division of the cells during the development of the embryo. Around 12-15 percent of confirmed pregnancies end in a pregnancy loss (miscarriage), but that percentage increases when the woman’s age (or the age of her egg) increases. It is estimated that 30-60 percent of all conceptions end in miscarriage prior to the woman even realizing she is pregnant. Unfortunately, the more pregnancy losses a woman experiences, the higher her risk of miscarrying the next pregnancy. However, overall, this risk remains under 50 percent per identified conception.
The age of the mother correlates with the the risk of miscarriage. Advanced Maternal Age (AMA), defined as a pregnancy in women 35 years or older, is thought to increase pregnancy loss due to the decreased quality of the eggs. The older a mother is, the higher her risk for having a child with genetic and chromosomal abnormalities, or experiencing a pregnancy loss due to chromosomal abnormalities in the embryo which are not compatible with life.
Sometimes, a woman’s uterus has an abnormality in the shape or contains polyps or fibroids. This distorts the cavity, leading to miscarriage. Some women are born with a misshapen uterus, and other women develop growths or fibroids over time. Sometimes, there is poor blood supply or inflammation in the uterus that also interferes with the pregnancy.
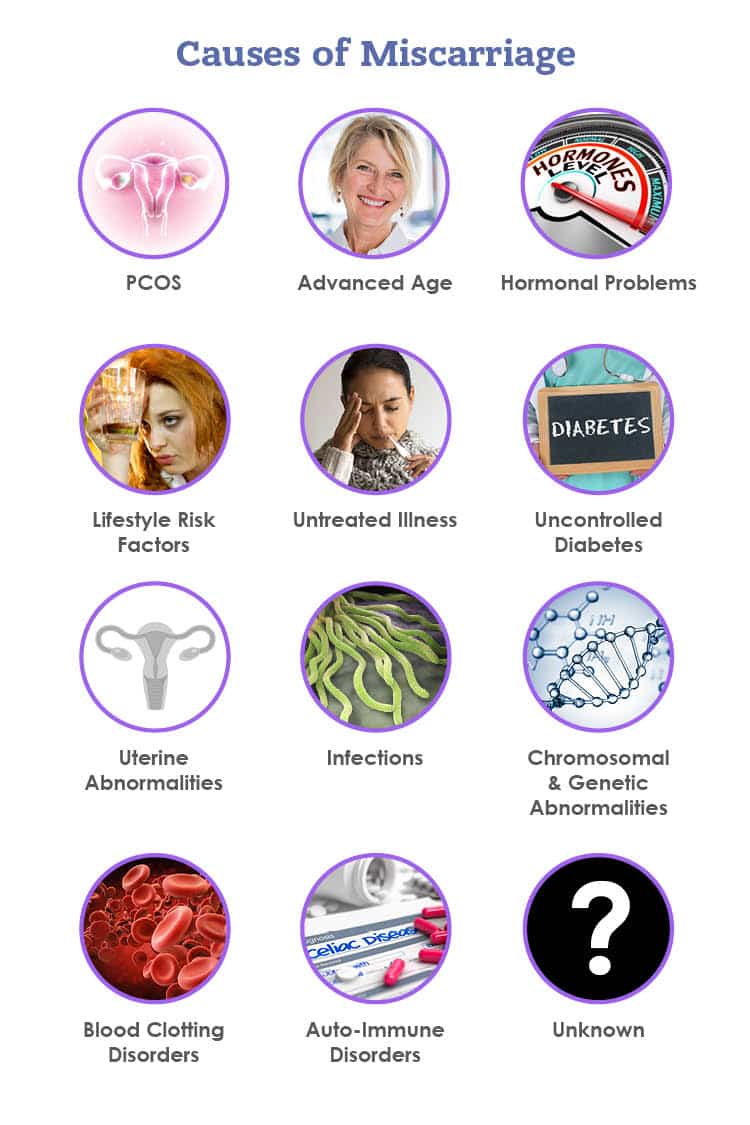
Auto-immune disorders, hormone abnormalities including PCOS (Polycystic Ovarian Syndrome), thyroid disease, diabetes, and other blood clotting disorders can increase the risk of pregnancy loss as well as blood clotting problems.
A common misperception is that stress, environmental factors, and occupations routinely affect pregnancy loss.
Hope for Couples Experiencing Repeated Pregnancy Losses
For couples who are trying to conceive a baby, the appearance of 2 lines on a home pregnancy test (HPT) represents joyful news signaling the beginning of a couple’s journey to becoming first time parents or increasing their family. When a miscarriage occurs, couples experience shock, disbelief and sadness. Pregnancy loss is far more common than most couples realize with the chances increasing with a women’s age. For women under the age of 30, the risk of pregnancy loss is 9 to 12%. The incidence of miscarriage triples for women after age 35 and approaches 50% per conception for women after age 40. Fortunately, the vast majority of women who experience a pregnancy loss will have a successful outcome with their next conception. However, for approximately 3% of couples, pregnancy loss becomes a recurring problem. For these couples, a double line on the HPT unleashes a roller coaster of emotions including fear and anxiety. Recurrent pregnancy loss (RPL) can affect both childless couples as well as those who have 1 or more healthy children. According to the American Society for Reproductive Medicine, couples who experience 2 or more pregnancy losses should undergo a medical evaluation. Testing can be helpful in elucidating a cause for RPL in up to 50% of couples.
The majority of miscarriages are due to chromosomal abnormalities in the embryo/fetus. Generally, embryos with too many or too few number of chromosomes (aneuploidy) can not develop into a healthy baby and result in abnormalities that lead to fetal death. Most of the time, aneuploidy is a chance event, the frequency of which increases with the advancement of a women’s age and, to a lesser extent, the male partner’s age.
For couples who experience more than 2 pregnancy losses, medical issues may be identified allowing intervention that can lead to a healthy baby. Reproductive Endocrine/Infertility physicians, specialized in the testing and treatment of RPL, can assist patients in identifying potential causes and prescribing treatments to improve a couple’s chance for achieving a successful pregnancy.
Disorders associated with RPL include chromosomal rearrangements that can be passed from the mother or father to their baby that results in the baby having an abnormal amount of genes, blood clotting disorders or antibodies that negatively affect embryo implantation or development of the placenta, abnormalities in the structure or shape of the uterus including the presence of scar tissue, polyps, fibroids or other congenital defects as well as hormonal abnormalities such as poorly controlled diabetes or thyroid disease. Additionally, lifestyle and environmental factors including obesity, cigarette smoking, use of drugs and consumption of alcohol and caffeine have been associated with increased risk for pregnancy loss.
The positive news is that treatments are available to assist couples who are experiencing RPL. For women who have experienced two pregnancy losses, seeking an evaluation can bring them closer to reaching their dream of having a healthy baby.
What can a Reproductive Endocrinologist, a fertility specialist do for pregnancy loss? I can GET pregnant.
Reproductive endocrinologists are indeed “fertility specialists” or experts in helping couples or women conceive. However, some patients do not realize they also specialize in problems sustaining pregnancies. Many of the same issues that cause female infertility, also affect the ability to carry a child to term.
At The Reproductive Medicine Group, a Tampa fertility clinic, one of our physicians who are board-certified Reproductive Endocrinologists will take detailed medical and family history, along with performing an exam. Testing will be ordered, including genetic screening of both partners. This looks for genetic and chromosomal abnormalities that may be causing the recurrent miscarriages. The uterus will also be evaluated. This can be done in several ways, but the most common ways are a saline sonogram (SIS) that can be performed at any of our 4 office locations or a hysterosalpingogram (HSG) or a saline sonogram that can be done in office at the North Tampa, Florida office. The doctor checks the shape of the uterus and for the presence of fibroids, polyps, or scarring.
A hysterosalpingogram or HSG is an X-ray that checks the function as well as the shape of both the uterus and the fallopian tubes, checking for blockage of the tubes. A saline sonogram can check the inside of the uterus, looking for abnormal shape or growths. Another method for evaluating the uterus is hysteroscopy, which allows the Reproductive Endocrinologist to directly visualize the inside of the uterine cavity.
A hysteroscopy is a minor surgical procedure where a tiny camera is inserted into the uterus through the cervix so that the doctor can clearly see the inside of a woman’s uterus. At this time, the infertility doctor (who is a surgeon) can safely remove:
- Polyps
- Fibroids
- A septum (abnormal shape of uterus)
- or remove scar tissue.
Bloodwork is ordered that checks for certain antibodies, like ones associated with blood clotting or auto-immune disorders. These antibodies may be associated with pregnancy loss or increased miscarriage rates. Sometimes, based on patient medical history, blood clotting factors.
Finally, and importantly, hormone function tests will be performed. These include thyroid, prolactin (another hormone that helps a woman make breast milk), and ovarian reserve tests. Ovarian reserve tests show how well the ovaries are functioning. Sometimes, when ovarian function is low, there are a higher number of eggs with genetic and chromosomal abnormalities.
Can recurrent pregnancy loss be treated?
Yes.
The vast majority of women will be able to get pregnant with proper treatments. Treatments are dependent upon the underlying cause of the miscarriages. These infertility treatments include:
- surgery to correct uterine abnormalities
- IVF (sometimes with PGT which screens for chromosomal abnormalities and birth defects in the embryo)
- medication to correct hormone imbalances, improve the uterine lining, or reduce blood clot formation.
Some couples can experience both problems getting pregnant as well as recurrent miscarriage. That’s why it’s important to seek testing and diagnosis from a Reproductive Endocrinology Specialist, who is an expert in conception and sustaining a pregnancy.
Choosing A Fertility Specialist
Now you know that an infertility diagnosis is defined as not getting pregnant after 6-12 months of unprotected intercourse. You also know infertility issues can be due to problems in the man, the women, both, or unknown factors. But the most important thing that you should remember is that INFERTILITY IS TREATABLE. Because infertility is a progressive disease, meaning it gets worse over time, it’s important to see a fertility specialist right away.
Have you been referred by your doctor to a “Fertility Specialist”? Were you advised by your family or friends to make an appointment with a “Reproductive Endocrinologist”? Or did you simply google your concerns and come looking for answers about getting pregnant or pregnancy loss?
However you came to find us, we are here to help. You can trust that you are in capable, expert hands to guide you through the process of creating your family.
The Reproductive Medicine Group is a team of fertility experts comprised of physicians, nurses, and staff who specialize in treating:
- infertility
- hormone disorders including PCOS
- recurrent miscarriage (pregnancy loss)
- preserving fertility through egg, semen, and embryo freezing.
Board- certified in OB-GYN with a sub-specialty board of certification in Reproductive Endocrinology and Infertility, our doctors are true fertility specialists. Our fertility clinic provides comprehensive service to offer you reliable and effective care in 4 convenient Tampa Bay locations: North Tampa (USF area), South Tampa, Brandon (which serves many patients from Polk and Manatee Counties), and Clearwater (which serves St. Petersburg, New Port Richey and Pasco County). Our services include:
- Ovarian stimulation
- Extensive fertility testing and diagnostics.
- Expert surgeries to treat other related disorders like endometriosis, fibroids, uterine abnormalities, ovarian cysts, and other fertility enhancing surgical procedures.
- Intrauterine insemination (also called artificial insemination or IUI)
- IVF (In Vitro fertilization) treatments
When choosing a Reproductive Endocrinologist for testing/ diagnosis, basic treatments, and especially for IVF (in Vitro fertilization) below are some good questions to consider about the fertility clinic, surgery center, and the team of fertility experts.

Our physicians are board certified Reproductive Endocrinologists, who are board certified in both Reproductive Medicine and Infertility and OB/GYN.
Learn more about our recent IVF Success Rates
The Reproductive Medicine Group has locations around the Tampa Bay area, 4 clinic locations within West Central Florida and a Surgery Center.
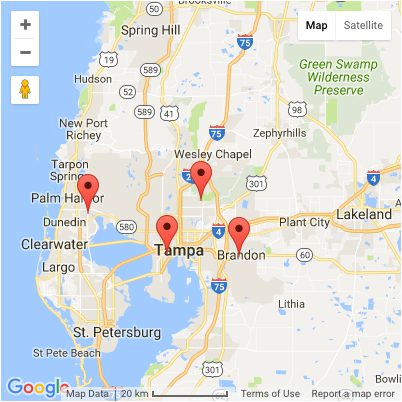
North Tampa
Convenient to Carrollwood, Lutz, Land O’ Lakes, Wesley Chapel, Temple Terrace and New Tampa. It is just down the street from the University of South Florida (USF) main campus, and close to Florida Hospital Tampa. (Convenient to I-75 and I-275 South or North if coming from other areas in Florida).
5245 E. Fletcher Ave. Ste 1, Tampa, FL
813-914-7304
South Tampa
Convenient to MacDill, Hyde Park, Downtown Tampa, Tampa Heights, and Seminole Heights, and the International/Westshore Mall area. This clinic is near Memorial Hospital.
2919 Swann Ave. Ste 305, Tampa, FL
813-870-3553
Brandon
Convenient to Riverview, Valrico, Fish Hawk, Seffner, Mango, Riverview, Apollo Beach, Plant City, and Lakeland. We even have patients come from Parrish, Bradenton, and Lakewood Ranch! This location is near Brandon Regional Hospital.
612 Medical Care Dr., Brandon, FL
813-661-9114
Clearwater
Our Pinellas county location serves St. Petersburg, Pinellas Park, Largo, New Port Richey, Hudson, Tarpon Springs, Safety Harbor, Trinity, and we even have patients come from Spring Hill and Brooksville! This center is near the Countryside Mall and Morton Mease Plant Hospital.
3165 McMullen Booth Rd. F-2, Clearwater, FL
727-724-0702
Learn more about the Insurance Plans that RMG accepts
To better understand your pregnancy odds, please click here for our infertility success rates.
For more information about infertility treatment costs, please follow this link.
The Reproductive Medicine Group offers personalized peer mentoring from previous and current patients.
Find out more about The Reproductive Medicine Group’s state of the art infertility surgical center located in Tampa, Florida.
Fertility Glossary of Terms
The staff at the Reproductive Medicine Group has compiled a list of frequently used terms that you will see throughout your treatment and on this website. Please use the following list so you may better understand the procedures and treatments offered.
- Advanced Reproductive Technologies (ART): Used to assist couples in overcoming infertility through the joining of the sperm and egg outside of the body and the transfer of resulting embryos. These procedures include: In Vitro Fertilization, Donor Oocyte IVF, Micromanipulation (ICSI and AH), Cryopreservation of embryos and sperm-related procedures.
- Aspiration: A method of removing eggs from the ovaries via a needle which is passed through the vagina into the ovary.
- Assisted Hatching (AH): A small opening is made in the shell of the embryo to improve the chances of implantation.
- Cryopreservation: A process that preserves embryos by freezing them for later implantation.
- Egg Donation: This procedure is utilized for women who lack good quality eggs or do not produce healthy eggs. Generally, egg development is stimulated in a younger woman, who donates the eggs which are then fertilized with the patient’s spouse/partner’s sperm. The embryo is then transferred into the woman’s uterus.