Home »
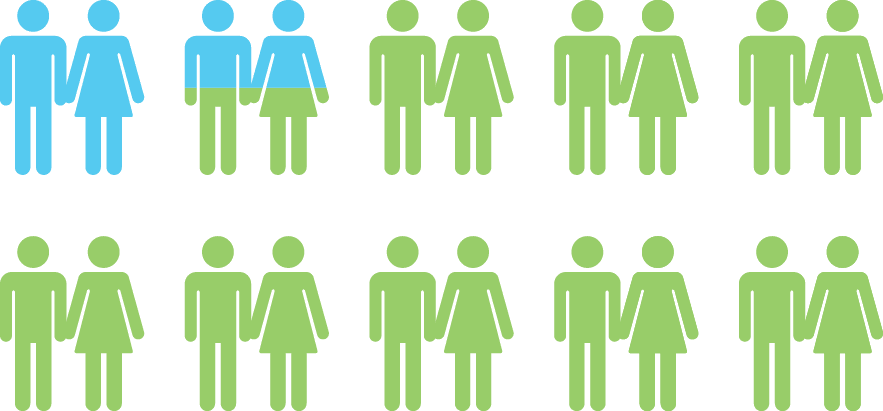
Approximately 15% of couples who are trying to conceive will be unsuccessful within a year of discontinuing all forms of contraception.
If you are among the more than 6 million couples in the U.S. who have not achieved a pregnancy after 6 months to a year, you could receive an infertility diagnosis. The recommendation for the first step in treating infertility is to undergo fertility testing of BOTH male and female partners with a Reproductive Endocrinologist. This type of specialist provides testing, evaluation, and infertility treatment.
Why Test/Timeline
Newer guidelines recommend that women ages 35 and above should undergo testing if they have not conceived after 6 months of discontinuing any form of contraception. At The Reproductive Medicine Group, we are fully equipped to explain, assess, diagnose and treat infertility regardless of whether the problem is simple or complex.
As discussed in Your Fertility, problems with fertility can come from either male or female issues, or even both. It is imperative that both partners be fully tested, to determine the problem. This is important so the correct, and most minimally invasive treatment may be used with success.
Although some couples have fears or concerns, making the decision to see a physician and initiate testing is the critical first step in overcoming fertility issues and achieving a pregnancy. Knowledge is power. After an initial consultation visit, the physicians at The Reproductive Medicine Group will recommend the appropriate tests based on your history. Basic fertility testing generally includes an assessment of the male through a semen analysis and assessment of the female through blood work and radiologic examination to determine hormonal status, egg health, uterine shape and fallopian tube health. Each of the tests are relatively simple and quick. While taking the first step by setting up a consultation appointment may feel overwhelming, it is the most important step in overcoming infertility, achieving a pregnancy and having a baby.
Fertility Tests for Women
Ovarian Reserve Testing
Loss of eggs or oocytes is one of the reasons the basis for lower fertility and higher miscarriage rates seen in women as they age. Decline in ovarian reserve begins in the early thirties, accelerates in the late thirties and plays a significant role in the increased incidence of infertility in the forties. The rate of this natural decline in ovarian oocytes varies among women. Some women will experience a decline in egg health in their 20’s while others remain fertile into their early 40’s. Tests to assess ovarian reserve are useful for both the physician and couple experiencing infertility as they provide a more complete understanding of the likelihood of a woman conceiving with her own eggs. However, there are limitations to all tests such that some women with poor or abnormal results may still conceive a healthy child with their own eggs while others with normal results could still have unhealthy embryos with continued infertility. Several tests are now available to assess egg reserve.
-
The most common test of ovarian reserve is the cycle day “3” FSH and Estradiol.
These blood tests can actually be drawn on day 2, 3, or 4 of the menstral cycle. FSH is a hormone produced by the pituitary gland in the brain, not by the ovary or the egg and as such, is an indirect measure of ovarian functioning. Although most widely obtained and studied regarding predictability of egg reserve, the test result can vary from menstral cycle to menstral cycle making the results less reliable. The current concept is that an abnormal result is indicative of decreased chances that a woman will conceive with IVF and takes president over prior or subsequent normal results. A normal day 3 fertile FSH level is generally <10 mIu/mL with the estradiol level <75pg/mL.
-
Anti Mullerian Hormone
– AMH is also a blood test reflective of ovarian reserve. Unlike FSH, blood work can be obtained at any time during the cycle and the level shows less cycle to cycle variability. AMH is generated within the ovary and therefore is considered to be a more direct measure of egg health; however, since it has been utilized to measure ovarian reserve more recently, it has not yet been adopted as ‘the gold’ standard for ovarian reserve testing. A normal value for most labs is greater than 0.7, although a value of 1.2 or above is considered optimal.
-
Antral Follicle Count (AFC)
– These tests are obtained using transvaginal ultrasound measurements usually early in the menstrual cycle. The size of the ovaries and number of visible immature follicles present early in the cycle has been demonstrated to reflect the number of eggs that have the potential to develop during a treatment cycle. Normal AFC is greater than 10.
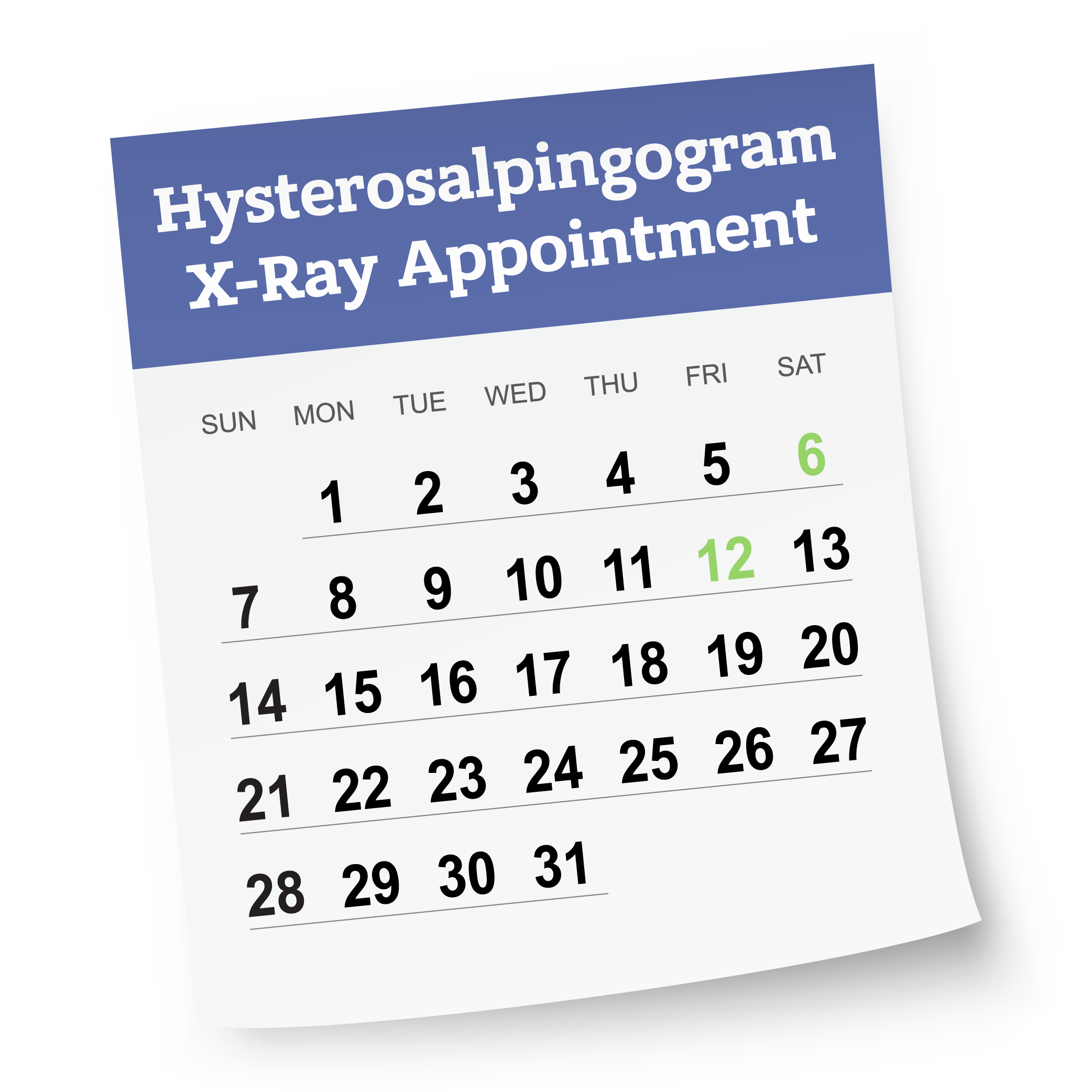
HSG – Hysterosalpingogram
This x-ray is useful in determining if the fallopian tubes and uterus are normally structured, and if the tubes are open. It is performed at our North Tampa office and should be done between the 6 th and 12 th cycle day. Call the office to schedule your hysterosalpingogram at the onset of your menses the month you will have the test performed.
The hysterosalpingogram takes about 15 minutes to complete, and may be associated with mild discomfort or cramping. You will be given a prescription for an antibiotic and pain medication when you schedule the procedure. You may have some mild bleeding or spotting afterwards. Should you experience bleeding heavier than a period, or a temperature above 100.4 degrees, call the office at which you are seen. If you are allergic to shell fish or iodine, or have had a prior reaction to x-ray dye, it is important that you inform the office when you schedule the procedure.
During the procedure, you will lay on the exam table in a position similar to when you are having a pelvic exam or pap smear done. Just as with the pap smear, a speculum will be placed. An antiseptic solution is placed onto the outside of the cervix and then a small catheter is placed into the cervical opening. Clear dye that contains iodine is injected through the catheter into the uterus while a special x ray called fluoroscopy is performed. This allows for visualization of the uterine cavity.
Within less than a minute, the dye will then enter the fallopian tubes if they are patent (open) and then spill out of the ends of the tubes. A cramping sensation may be felt as the dye enters and passes through the tubes but this should be brief, especially if you take the prescribed medications prior to the examination. If there is an abnormality in the shape or distribution of the dye within the uterine cavity, you may be advised to schedule a special ultrasound examination of the uterine cavity (saline infusion sonogram/SIS/hysterosonogram). If abnormalities are found in the fallopian tube evaluation, you will need to schedule a consultation appointment with your physician to review your options.
Preconception/Prenatal/Genetic Screening
Preconception, prenatal, and genetic screening are key steps in identifying women at risk of transmitting infections or genetic problems to their babies. Screening tests often allows for timely initiation of interventions to prevent these problems from occurring. Without this information, we cannot identify those problems or help patients have the best chances for a healthy pregnancy and baby. We highly recommend these tests for ALL infertility patients.
Prenatal Screening Includes:
- Complete Blood Count (CBC)
- Hepatitis B
- Hepatitis C
- HIV (AIDs)
- RPR (Syphilis)
- Genprobe (Gonorrhea/Chlamydia)
- Blood type and Rh neg or positive
- Rubella titre (German Measles)
- Varicella titre (Chicken Pox)
Genetic screening checks for major health issues that a patient may carry in their genes, which they would not realize they had. A patient often will not have a known family history of disease when they are a carrier. It is important to test each female patient to see if she is a silent carrier of these conditions. These conditions can also affect the embryo’s implantation and growth, leading to pregnancy loss or inability to become pregnant. For the highest chance of a healthy pregnancy and live birth, it is important that every fertility patient have a genetic carrier screening. This is done with a simple blood draw that is sent to Myriad Clinical Laboratory for analysis.
The Reproductive Medicine Group physicians recommend genetic Screening (through Myriad Clinical Laboratory). It is called the Foresight Carrier Screen and is used to detect mutations associated with more than 175 serious conditions that fall into one of the following categories:
- Conditions where early treatment can make a difference (such as PKU)
- Conditions that cause intellectual disability (such as fragile X syndrome)
- Conditions that shorten lifespan (such as Bloom Syndrome)
- Conditions where there are limited to no treatment options available (such as Tay-Sachs disease)
A full list of genetic conditions screened is available at myriadwomenshealth.com/foresight/diseases.
Saline Infusion Sonogram (SIS)
A saline infusion sonogram (saline sonography) is routinely performed to make sure that the endometrial cavity (inside of the uterus) appears normal. Benign uterine growths, such as endometrial polyps or uterine fibroids, may develop in the cavity and create an environment that is hostile for embryo implantation. Scar tissue may also be identified with the saline infusion sonogram. This procedure may be done as part of an evaluation for recurrent pregnancy loss or done prior to an IVF cycle. It may also be done to evaluate causes of irregular or very heavy menstrual cycles and some types of chronic pelvic pain. The saline infusion sonogram is scheduled early in a menstrual cycle, just after your period stops but before ovulation – usually between days 5-12 of the cycle.
The procedure is simple and usually takes 10 to 15 minutes to complete.
- A speculum is inserted into the vagina and the cervix is cleansed with an antiseptic solution.
- A special catheter approximately 1mm in diameter (about the size of a single strand of spaghetti) is inserted and slides through the cervical canal.
- The ultrasound probe is placed in the vagina.
- Sterile salt-water solution (saline) flows through the catheter into the uterine cavity. This distends the endometrial cavity and allows the physician to see the entire cavity on the ultrasound monitor. You may experience mild cramping at this point.
- Several images of your uterus will be taken during the procedure, pictures of your ovaries may also be taken.
- You will need to schedule an appointment with your physician to discuss any abnormalities that are seen during the procedure.
After the procedure, you may continue to have mild cramping for a few hours. You may also experience light spotting or watery discharge for as long as 24 hours after the procedure. You should refrain from intercourse for approximately 48 hours. If any symptoms other than those listed above are noticed, please call the office at which you are seen.
Semen Analysis – Male Infertility Test
Approximately 40% of infertility in couples is attributable to male factors, and another 20% of infertility cases involve both female and male issues. Some of the factors may be suspected or known to the couple prior to attempting conception, while most might not be anticipated. Certain medical conditions or exposure to toxins can lead to damage to the sperm producing cells or affect release of the sperm. Conditions such as undescended testes not corrected within the 1 st year of life, cystic fibrosis, diabetes, cancer or other chronic illnesses may affect sperm production and/or release. Exposure to chemotherapy, radiation, use of supplements containing androgens including Testosterone, DHEA and gym work out aids, certain herbs, over the counter medications or prescribed medications can inhibit sperm production. In some cases, toxin exposure or ingestion can permanently destroy the cells that produce sperm resulting in sterility. The use of hot tubs, alcohol ingestion (in excess of 7-10 drinks/week), tobacco and marijuana all have adverse effects on sperm production and function. However, in many cases, there are no known exposures, health issues or family history to account for abnormalities found at the time of a semen analysis.
Infertility is associated with a female problem in 40% of couples, a male problem in 40% and either a combination of problems and/or unexplained in 20% of couples.
Given the significant percentage of male infertility cases associated with sperm abnormalities, a semen analysis should be among the first tests performed in couples experiencing unexplained infertility. As many minor, transient conditions can affect the sperm, if an abnormality is detected, generally a second semen collection and analysis is recommended to confirm the initial result.
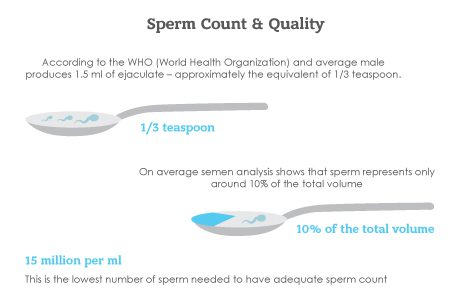
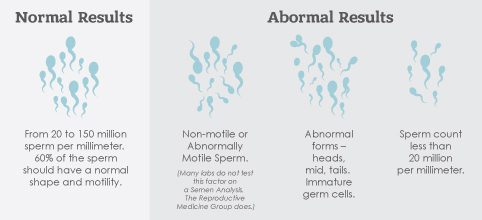
The evaluation of the semen sample includes numerous factors including concentration (number) of sperm, motility (percentage of sperm moving or swimming) and morphology (sperm shape). Significant abnormalities in any of these parameters will decrease the likelihood of a sufficient number of sperm being able to reach or penetrate the egg.
If significant abnormalities are detected on repeated semen analysis studies, a consultation with a urologist who has special training in male infertility may be recommended. Blood work, a physical exam and possibly a scrotal ultrasound could be suggested.
Treatment options vary depending upon the results of the evaluation and degree or severity of the abnormalities found on the semen test. The most important initial steps include eliminating toxin exposures including alcohol, tobacco, illegal drugs and any form of male hormone precursors or supplements, avoiding excess heat exposure and maintaining a healthy diet including foods rich in folic acid and antioxidants (green leafy vegetables, whole grains as well as colorful fruits and vegetables). A urologic evaluation may reveal a problem that can be treated medically or surgically. If alterations in lifestyle do not improve semen parameters and no medical or physical problem contributing to the poor sperm qualities can be identified, then treatment options can include sperm concentration and placement into the uterus (intrauterine insemination/IUI) or in vitro fertilization (IVF) with injection of a single sperm into each egg (intracytoplasmic sperm injection/ICSI).
This is the first, and most important, male infertility test. Abnormalities in semen parameters (male factor) contribute to infertility in approximately 40% of couples. In many cases, this will be the only infertility test required for the male. Sometimes, the semen analysis will need to be performed more than once.
The specimen is collected by masturbation into a collection container after abstaining from ejaculating for 2-5 days. It is best if it can be collected at one of our office laboratories, however, if that is not possible, it may be collected at home and brought to our laboratory within 1 hour of collection time. Be sure to record the time of collection. After collecting the specimen, keep it at body temperature by placing it in your shirt pocket or wrapping it in a towel. Do not expose the specimen to extreme temperatures such as air conditioners or heater vents. More information will be provided when the procedure is scheduled
Many aspects of the semen are examined during the semen analysis. Assessment of volume (normal is > 1.5cc), concentration/count (normal is > 20 million per cc), motility/movement (expect at least 40% to be moving) and morphology/sperm shape (need to have a t least 3% with normal shape according to strict criteria) is made. In addition, viscosity (thickness/ability to liquify), presence of bacteria or white blood cells and pH are observed.
If one or more parameters are abnormal, a repeat analysis will be required. If repeat test results are significantly abnormal then a urologic evaluation may be recommended.