Home »
Understanding IVF (In Vitro Fertilization)
What is in vitro fertilization?
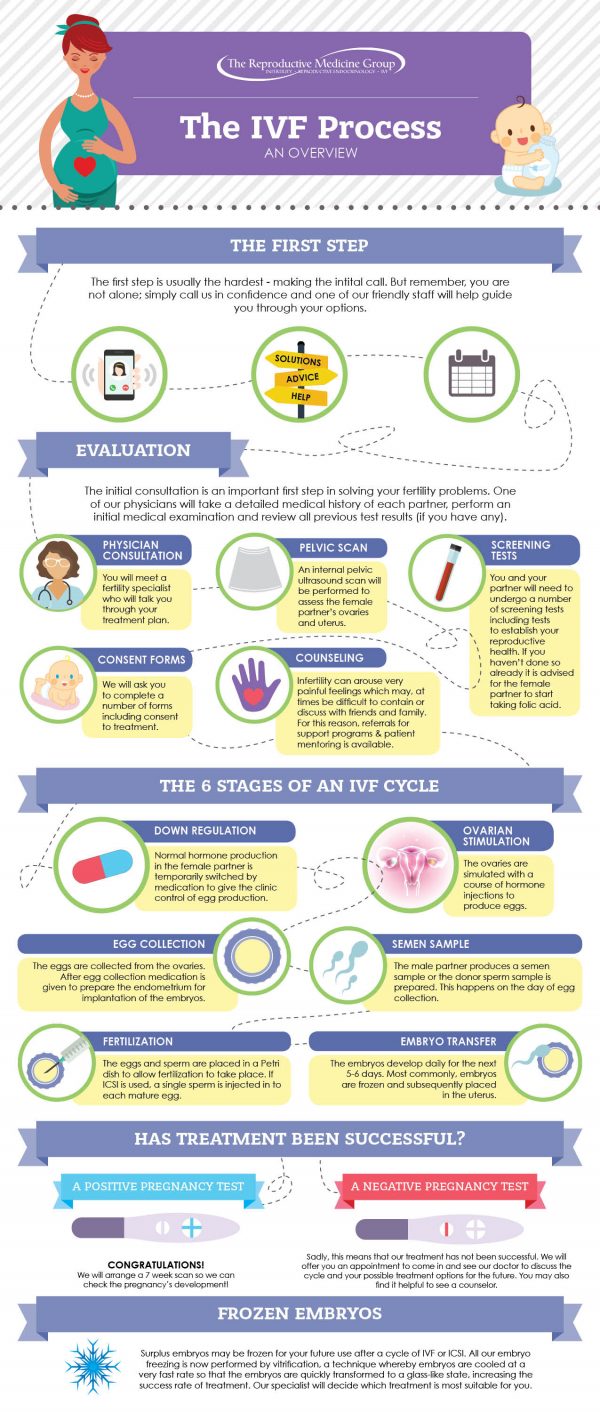
A very basic explanation of IVF, which is an Assisted Reproduction Technology (ART) procedure is:
- Extracting a woman’s eggs
- Collecting a man’s sperm sample (or purchasing donor sperm)
- An embryologist manually combining egg and sperm in a laboratory to create embryos
- Implanting an embryo into a woman’s uterus.
When many people think of fertility treatments, they think of IVF (In Vitro Fertilization). It’s important to realize, however, that most patients get pregnant with less invasive fertility treatments. Only 10-15 percent of patients require IVF treatment in order to have a successful pregnancy. Here are some top questions you may have when first researching your treatment options.
There are several instances where IVF may be appropriate. A Reproductive Endocrinologist will do a variety of tests to evaluate the right treatment for you. Some couples or individuals who may be recommended for IVF are:
- Women with tubal infertility factor (tubes blocked or non-existent)
- Women with endometriosis
- Women who have PCOS (Polycystic Ovarian Syndrome)
- Men who have poor or absent sperm
- Women who are using donor eggs via egg donation
- Couples who are at risk for known genetic disorders
If a woman’s egg quality or reserve is too low for conventional IVF due to age or other factors, donor eggs may be successfully used for IVF.
IVF has several set stages, but it’s not always a straightforward process. It may not go the same for every couple. Every infertility treatment plan is unique, fertility problems are different, and adjustments are made through each cycle to give couples the best chance to conceive.
Imagine IVF being a road trip to a destination. Just like any other trip you may take, there is certainly a route you will take, but there will also be other variables that you may experience. Will there be traffic? Are there any detours? Will there be any other unexpected delays?
So each couple begins their IVF journey with the same destination in mind, but each “trip” will be different.
Step 1:
Patient/couple makes a decision with their physician to pursue IVF. This is after completing fertility testing and discussing appropriate infertility treatment options.
Step 2:
Couple (or patient) begins their IVF preparation education.
Step 3:
After payment and consent signing, stimulation begins. During stimulation, there may be several outcomes.
Multiple follicles develop and several “good” eggs are retrieved – then you move along to fertilization.
OR
There are not enough follicles or “good” eggs to proceed. You must go back to stimulate again. The doctor will make adjustments to your cycle. If you must go back to stimulation, it does not mean your journey is over. There have been many patients who, after adjustments are made, stimulate successfully. In this scenario, you are slightly delayed in your journey, but you are still on your way.
Step 4:
Embryos are created. Here are the possible outcomes:
You have one or more “good” quality embryo(s). You move on to PGT (if recommended by your doctor). Embryos are frozen and transferred once genetically healthy embryos have been identified.
OR
You have one or more quality embryo(s). You do not choose PGT. Embryos may be frozen and stored for future use and/or an embryo may be transferred into the uterus during that cycle.
OR
You do not create any quality embryos. Adjustments are made by your doctor, and you head back to stimulation. Once again, although slightly delayed, you are still on you way to your pregnancy destination.
Step 5:
Transfer Time! What happens next? Your best embryo will be transferred into your uterus! Possible outcomes are:
Pregnant – Yay! Embryo implantation is successful! You are released to your regular OB/GYN after 8-12 weeks. Any additional frozen embryos will be stored for future use.
OR
Not Pregnant, with more stored and frozen embryos – Again, you are detoured, but not dismayed. Your journey continues, the doctor will make adjustments, and you go back to Transfer.
Not Pregnant without stored and frozen embryos – You will need to go back to stimulation. Again, you are delayed, but your journey is still moving forward. The doctor will make adjustments, and you will re-enter the process at stimulation.
For most couples, this is a 4-6 month process. This is mainly due to most steps having to align with a menses (period).
This varies by several factors. First of all, live birth rates are preferred over pregnancy rates, however, the data takes longer to report, due to the time of gestation.
Typically, our doctors encourage a single embryo transfer for many reasons. The main reason is being a goal of a healthy pregnancy and a live birth.
On average, the multiple birth rate (twins) is just under 13% (36/287).
Again, there are many variables that affect cost, primarily insurance coverage and specific treatment plan requirements.
Click here for IVF Insurance Coverage
Long-term studies have shown no ill effects for children born via IVF.
IVF can be performed based on ASRM recommendations, up to age 55 if including the use of donor eggs. If egg quantity or quality is too low, donor eggs may be used for women of any age group.
According to the ASRM, gender selection for non-medical reasons is highly controversial and raises numerous ethical concerns including: gender bias, sex stereotyping, and issues of social justice. Given the ethical controversies and potential repercussions, The Reproductive Medicine Group offers gender selection for only medically indicated reasons.
In many cases, it can be. Another option for some patients, if appropriate, is tubal reversal.
Please consult with one of our physicians to explore which treatment path is right for you.
Table of Contents
IVF Procedure Details
In Vitro Fertilization is the process by which eggs (oocytes) are retrieved from the ovary, fertilized by the sperm in the laboratory, and cultured into early embryos. The embryos are then transferred into the uterus. Since multiple eggs are desired in order to enhance the likelihood of developing one to three healthy embryos, stimulation with injectable fertility drugs, (gonadotropins) are usually required. Frequent monitoring is necessary with sonograms and blood tests. When these diagnostic methods indicated that the time is appropriate, a trigger injection is taken to mature the eggs. The eggs are retrieved from the ovary just before they are ready to be ovulated. This is usually about 36 hours after the trigger injection.
For IVF, the eggs are usually retrieved by ultrasound guided needle aspiration through the vagina. Transvaginal egg aspiration is done using intravenous anesthesia, which is administered by an anesthesiologist. This out-patient procedure is performed at The Reproductive Medicine Group’s IVF and Surgery Center.
After aspiration, the embryologist determines the number of eggs obtained and classifies them as mature, immature, post mature or degenerative. Immediately following the egg aspiration, the spouse/partner will meet with the IVF Andrologist to provide a semen specimen. The sperm is then processed in our IVF lab in Tampa, Florida. The sperm and eggs are placed in a dish and fertilization takes place (in vitro) outside the patient’s body in the laboratory. The fertilization process takes approximately 10-20 hours. Embryos are then cultured for 5 days before being replaced back in the uterus by a simple technique much like intrauterine insemination or cryopreserved (frozen). Prior to embryo cryopreservation, a few cells may be removed for genetic screening.
Embryo transfer occurs on day 5 at The Reproductive Medicine Group’s IVF and Surgery Center. Embryos are carefully placed into a special catheter and inserted into the uterine cavity. Generally, 1-2 embryos are transferred back into the uterus depending on the patient’s age, embryo quality and physician recommendation. The Reproductive Medicine Group strives to transfer the lowest number of embryos possible to reduce the risk of multiple pregnancy but maintain the best chances for conception.
A serum progesterone level is checked several days after a completed IVF cycle, and the first pregnancy test is approximately 10-14 days following the IVF transfer procedure.
As with many clinics throughout the U.S., patients planning to undergo IVF with The Reproductive Medicine Group will attend an evening IVF group class during which time the IVF procedures and protocols will be explained in detail. These classes are given by one of the RMG physicians and currently are held in the evening, the 3rd Tuesday of every month. A schedule of classes is posted in each RMG office.
Following the class, the couple will have an appointment to have the woman’s uterine cavity length measured, “mock transfer” and to sign consent forms. You should have a full bladder for the “mock transfer”. During that appointment, the physician will review information about IVF and answer your questions. The number of embryos to be transferred and plans to freeze embryos of high quality beyond the number to be transferred will be discussed at that appointment or the decision to perform genetic testing on the embryos or freeze all of the embryos for subsequent transfer will be discussed at that appointment. (It is critical that both you and your spouse read the IVF consent forms prior to that appointment!) The consent forms are extremely detailed and contain critically important information. Please do not leave that appointment without having all of your medical questions regarding IVF addressed.
You are expected to pay all fees not covered by your insurance at that appointment as well. As such if you have not received your bill, please contact the billing office prior to your appointment.
After your mock transfer/consent form signing consultation appointment, if your protocol includes down regulation with a birth control pill, you should be sure to pick up your pill pack. You are to call the ART nurse with the onset of your menses. You will be instructed when to begin your birth control pill and an appointment will be set up with the IVF nurses for you and your spouse to learn how to administer the IVF medications as well as to receive your personalized, detailed calendar which outlines expected appointments and timing of your medications.
You will begin your IVF stimulation medications according to your calendar after that appointment. Once you begin your stimulation medications, you will come into the office periodically for blood work and ultrasounds. These appointments are in the early morning usually between 7:30a.m. and 9:00a.m. The results will be ready in the mid afternoon and reviewed by the physician who will determine what your medication dose will be and when you will need to return for further monitoring. The IVF nurse will then contact you with instructions. For your convenience, monitoring is performed during the weekdays at all 4 of our locations. On weekends/holidays, monitoring is performed only at the North Tampa office. Oocyte (egg) stimulation medications (gonadotropins) are generally taken for 8-12 days (this does not include the days using the birth control pill).
When the blood work and ultrasounds (sonograms) suggest that several eggs should be mature, you will be instructed as to the time to take the trigger injection. Approximately 36 hours after the injection, the egg aspiration procedure will occur. Several days prior to the egg aspiration procedure, you will have a pre-op appointment with your doctor. You will have the opportunity to ask your doctor any additional questions you may have and will receive prescriptions for pain medication to use if needed, after the egg aspiration and for valium to be used on the morning of the embryo transfer.
You will report to the RMG IVF/Surgery Center at the instructed time on the morning of your egg aspiration. You are to have nothing to eat or drink beginning midnight prior to your aspiration procedure. This includes water, gum, candies and tobacco (all patients MUST discontinue tobacco at least 3 months prior to their IVF cycle). You may brush your teeth.

Upon arrival to the IVF Center, you will be admitted and an IV will be started. Your partner/spouse may be with you until you go to the operating room. You will be seen by the pre-op and OR nurses, the anesthesiology physician and the RMG physician who will perform the procedure. Once in the OR, you will receive medication through your IV to make you drowsy and then asleep. You will not feel any pain. The procedure takes 15 – 20 minutes. You will be returned to the post-op area. Once you are awake, your partner/spouse will be asked to produce the semen sample. If your spouse has difficulty producing a specimen, PLEASE inform your physician or the IVF nurses in ADVANCE (at least a week if not more prior to the aspiration procedure) so we can arrange to have his sperm collected and cryopreserved in advance when he will feel less pressure. As this incurs additional cost, we do not routinely recommend freezing sperm in advance. Men who have extremely low counts and some men undergoing retrieval of sperm from the testes will have their sperm cryopreserved prior to the IVF cycle.
The sperm and the eggs are united in the petri dish several hours after the egg has been retrieved. Assessment for fertilization is performed the following day. You will be contacted as to the number of eggs that successfully fertilize. Usually, approximately 70% of mature eggs fertilize but this can vary depending on the health of the eggs and sperm.
The embryos will be incubated, undisturbed for an additional 4 days and reassessed on the 5th day post retrieval. Embryos that reach the blastocyst stage by day 5 may be transferred into the uterus or biopsied for genetic screening and then frozen (cryopreserved). Those that do not reach blastocyst stage by day 5 will be re-evaluated on day 6 and biopsied and then frozen if they reach the blastocyst stage.
On the morning of your embryo transfer, you will fill your bladder, take your valium pill as instructed and report to the RMG IVF/Surgery Center at the time assigned to you. You will be admitted, speak with the nurse and the physician will discuss the quality of embryo(s) to be transferred into the uterus. The number of embryos will be based on the grid previously discussed and determined at your consent form signing appointment. Your spouse/partner may accompany you throughout the procedure.
You will walk to the transfer room through the OR area (your spouse will be walked through the non-sterile hallway and meet you in the transfer room). Once in the transfer room, you will be asked to reverify your name and the number of embryos to be transferred. The procedure will be performed the same way the mock transfer was done by your doctor previously. An ultrasound will be performed while the physician places the transfer catheter and the embryos are inserted into the uterus. If your bladder is appropriately filled, you may be able to see the tip of the catheter on your smaller viewing screen. The lining closes around the embryos and, as such, you do not need to worry about the embryos falling out when you stand up or empty your bladder.
Many factors determine why some embryos implant while others do not. Embryo implantation success rates are directly related to the age and quality of the woman’s eggs. At The Reproductive Medicine Group it is our goal to give our patients the best chance for conception.
The Use of Assisted Hatching in IVF
Assisted hatching through micromanipulation has been shown to increase the IVF embryo implantation rate of embryos that are being thawed for a frozen embryo transfer cycle. Even if sperm – egg interaction and embryonic development proceed normally, attachment of the pre-embryo to the uterus must still occur.
A layer covering the egg called the zona pellucida performs many crucial functions in the process of fertilization and development. However, in order for the embryo to implant into the uterine wall, it must hatch out from its zona pellucida with the help of substances produced by the embryo.
A number of findings suggest that human IVF pre-embryos sometimes lack the ability to thin and hatch through their zona pellucida. The pre-embryo is held by a micropipette while a specialized laser beam is utilized to create a small opening in the zona pellucida.
The Impact of IVF on Male Infertility
How can IVF “treat” male infertility?
Intracytoplasmic Sperm Injection (ICSI) enables men with poor sperm quality to father children. ICSI is used when the male has a very low sperm count, if sperm motility is poor, or if there is a low percentage of normal shaped sperm. It is used in some cases of unexplained failed fertilization in a prior IVF cycle. It is also used for sperm obtained through TESE (testicular extracted sperm) and for all cycles involving PGT (pre-implantation genetic testing).
In the ICSI procedure, a microscopic hole is placed in the egg membrane with an instrument that resembles a needle. A single sperm from the male is inserted into the egg.
There is no difference between the offspring produced by ICSI and those conceived by other methods. There is now broad, successful, clinical experience with hundreds of ICSI patients and their children. Embryologists receive advanced training to enable them to perform this delicate procedure.
Can a man who can’t ejaculate healthy sperm still produce enough sperm for IVF?
Even in men with no sperm seen at the time of semen analysis, there may be sperm within the testes. This sperm can be removed by aspiration from the testes or epididymis in procedures called TESE (testicular sperm extraction) or MESA (microscopic epididymal sperm aspiration). TESE and MESA procedures combined with ICSI allow many men, previously considered sterile, to produce children.
What happens if I make multiple embryos in my IVF cycle?
Getting Started
Appropriate medical testing is required prior to scheduling your in-vitro fertilization cycle. Results of the screening tests will allow your physician to select the most appropriate therapy and protocol to maximize your chances of becoming pregnant. The following outline is designed to give you an overview of the preliminary ART process.
Initial evaluation with your physician:
Includes a comprehensive review of your medical history, past records, and a current physical exam.
- Please be sure to bring copies of your records, x-rays, prior surgical reports and laboratory information to your initial visit. If you have had an IVF cycle at another clinic, please bring in your cycle stimulation sheets and embryo information.
- As you may spend time not only with your physician but also with our nurses and counselors, please allow up to 2 hours for your initial visit.
Requirements for patients undergoing ART:
- Attend a virtual on-demand IVF education webinar. Your IVF Coordinator will work to get you enrolled for the class.
PLEASE NOTE: The use of donor eggs is recommended for patients undergoing IVF who are beyond the age of 43.
Prior to your consent signing appointment, please review:
- ART Consents which include: In-Vitro Fertilization, ICSI Treatment, Embryo Biopsy for PGT, and Embryo Cryopreservation, which can be found on our website. You may require additional forms depending upon your specific procedure.
- Financial Worksheet provided by our Financial Counselor/Business Office detailing professional fees, embryology fees, facility fees and estimated cost for medications costs.
- General information published by The American Society for Reproductive Medicine (ASRM).
- Updated pregnancy rates from our program.
At your consent signing appointment with your physician:
You and your physician will finalize your treatment plan.
- Review and sign consent forms.
- If you are going to have an embryo transfer, your physician may perform a Mock Trial Transfer to measure the uterine cavity. You will need to have a full bladder for this procedure.
- Payment of remaining fees for expected patient responsibility is due at the time consent forms are signed.
Attend Patient Education Night:
Patient education nights are held the third Tuesday of every month, addressing general information concerning the ART program.
Meet with ART Coordinators:
- You and your partner will have a consult visit with one of our ART coordinators to review your specific protocol, discuss what to expect during your ART cycle, receive your prescriptions and get detailed information regarding your medications, injection techniques, and cycle calendar.
- The ART Coordinators are available for your questions and to provide support during your IVF cycle.
It is our ultimate goal to help you become pregnant with a healthy child!
ART Program and Laboratory Information

The Reproductive Medicine Group is a LEADER in the treatment of Infertility in the Tampa Bay region. ART therapies, most common of which is in vitro fertilization (IVF), assist couples in overcoming fertility issues through the joining of the sperm and eggs outside the body and then transferring the resulting embryo into the uterus. The ART program is comprised of dedicated physicians, nurses, embryologists and andrologists. Our ART Laboratory is located adjacent to our Surgery Center in North Tampa.
The RMG/ART Laboratory is fully accredited by the College of American Pathologists (CAP) in the areas of andrology and embryology. This accreditation indicates that the RMG/ART Laboratory belongs to an exclusive group of laboratories throughout the country that meet the highest standards of excellence as recognized by their peers. The accreditation process includes an evaluation of all aspects of quality in the laboratory: Methodology, reagents, medical equipment control, specimen handling, procedure manuals, reports and proficiency testing, personnel and the overall management principles that distinguish a quality laboratory. The CAP is an advocate for high quality and cost effective medical care.
The RMG/ART Laboratory also participates in the biannual proficiency testing by The American Association of Bioanalysts. This comprehensive external quality control program satisfies the proficiency testing requirements for Clinical Improvement Amendments, Commission on Office Laboratory Accreditation, Health Care Financing Administration, Joint Commission on Accreditation of Healthcare Organizations, CAP, and most state agencies.
The Reproductive Medicine Group ART Laboratories Inc. in Tampa, FL has been awarded accreditation by the Accreditation Committee of the College of American Pathologists (CAP), based on the results of a recent onsite inspection in December, 2010. The Reproductive Medicine Group was advised of this national recognition and congratulated for the excellence of the services being provided. RMG ART Laboratories Inc. is one of more than 7,000 CAP-accredited laboratories worldwide. The CAP Laboratory Accreditation Program, begun in the early 1960s, is recognized by the federal government as being equal to or more stringent than the government’s own inspection program. This stringent inspection program is designed to specifically ensure the highest standard of care for all of our patients.
IVF FAQs
• Smoking: Stop smoking before ovulation induction begins. It is best to discontinue tobacco at least 3 months prior to an IVF cycle. If you cannot stop “cold turkey”, seek the care of your primary care physician. By products of tobacco have been demonstrated to be toxic to the oocyte (egg). Numerous studies have also demonstrated that smoking during pregnancy results in reduced birth weight and fetal compromise. There is some data that smoking can also lower pregnancy rates. We strongly recommend that all women, especially those undergoing fertility treatment, cease smoking.
• Drinking: Alcohol is a drug, and should be avoided during infertility treatment and pregnancy. Please do not drink alcohol from the time fertility medications are initiated until the pregnancy test.
• Medications: If you are taking any medication, prescription or over-the-counter, please inform your physician. Some medications may interfere with the fertility medications prescribed, some are not safe to use before an operation or medical procedure, and others might interfere with ovulation or pregnancy implantation. A prenatal or multivitamin will be prescribed; if you are not taking a vitamin with folic acid, please inform the ART nurses. Also, please note: DO NOT USE HERBAL SUPPLEMENTS DURING YOUR IVF CYCLE.
• An IVF cycle can be an emotional and stressful time for you and your partner. It may be helpful to have supportive personnel to speak to, such as friends and family, a clergy member, or a psychologist/therapist.
• Heavy exercise such as aerobics, jogging, weight lifting etc. are prohibited during ovarian stimulation and until the pregnancy test results are known.
• Acupuncture is permitted prior, during and after your IVF cycle but herbal supplements are absolutely prohibited.
On the day before the oocyte (egg) retrieval, oocyte culture dishes are labeled with the patient’s name, date of birth, and ART identification number. The number and size of the ovarian follicles determines the number of dishes prepared (one dish for each large follicle). The dishes are filled with a rinsing fluid in the outer well for removing blood and other extraneous cells from the egg, and a nutrient fluid for the culture of the egg is in the center well.
The dishes are then placed in the embryology incubator for warming to body temperature. The incubator also adjusts the pH of the culture media to the human body. A large amount of rinsing media is equilibrated in the incubator. Media is also equilibrated in the andrology laboratory for processing of the sperm.
One of the more important and useful IVF laboratory instruments is the mobile IVF chamber. It is a pediatric isolette (incubator) on wheels that has been modified to contain a scanning microscope. Prior to the egg retrieval it is warmed to body temperature and put at the normal neutral pH of the culture dish media. These conditions avoid any abrupt changes the eggs might encounter outside the body. The chamber has two small doors on each side. The embryologists place their hands on one side to identify eggs and move dishes. The OR nurse uses the opposite doors to pass test tubes containing the follicular fluid to the embryologist.
Upon arrival in the operating room the patient’s identity is verified by the embryologist, physician, and safety nurse. They also verify that the culture dishes are correctly labeled. At the time of surgery the mobile chamber is loaded with the equilibrated petri dishes for receiving the follicular fluids.
The physician aspirates the fluid from the ovarian follicles into a test tube. A nurse passes the test tube, through the IVF isolette chamber door, to the embryologist. The embryologist then dispenses the fluid into a large dish and rapidly scans it under the microscope. The egg complex is usually visible to the naked eye, but microscopic verification is always done. The oocyte is removed from the large dish by pipette, rinsed in the outer well of the culture dish and placed in the center well for culture and the addition of sperm (insemination). The presence of an egg in the follicular fluid is reported to the physician.
After all of the eggs have been aspirated, the mobile chamber is moved to the embryology laboratory for a more critical assessment of the oocytes, insemination with sperm, and culture.
The maturity and health of oocytes are assessed after an incubation period. Oocytes are graded as mature, intermediate, immature, or degenerate. Oocytes judged mature are incubated 1 to 4 hours before insemination. Less mature oocytes are incubated until they reach maturity, and then inseminated. Approximately 100,000 motile sperm are added to the media surrounding the oocyte in the center well of the culture dish. Dishes containing egg and sperm are then returned to the main embryology incubators for culture.
The male will be asked to collect a semen sample after the oocyte aspiration. The andrologist escorting him to the collection room will identify the patients partner from his identification bracelet prior to collection and will write both names on the outside of the specimen container after collection. The partner will be asked to verify that both names are correct.
Approximately 30 minutes after collection, when the semen liquefies, a semen analysis is performed. The sperm is prepared for insemination.
Twenty to twenty-four hours after retrieval, the oocytes are transferred to fresh dishes that were equilibrated on the day of retrieval. Oocytes are then microscopically examined for pronuclei formation, the sign of fertilization. The pronuclei are the decondensed DNA of sperm and egg nuclei. They appear microscopically as two light spheres within the egg. Oocytes possessing more than two pronuclei are discarded. These abnormal fertilizations are typically naturally aborted.
Fertilized oocytes are returned to the main embryology incubator for 24 hours. At that time the embryos are transferred to fresh dishes where the cell stage and overall health of the embryos are microscopically evaluated. The embryos are either transferred on day 3 or placed into new dishes with a specialized culture media to allow for progression to the blastocyst stage.
The blood pregnancy test is performed 14 days after the egg retrieval.
If pregnant, you will be asked to return to the office for repeat blood work and eventually an ultrasound to ensure an ongoing successful pregnancy. After a fetal heartbeat has been confirmed, patients are referred to an obstetrician for the remainder of the pregnancy.
Usually we ask that patients wait one or two complete menstrual cycles before beginning another ART cycle. Sometimes tests are required that may delay subsequent cycles.
A high risk OB is only needed when there are complications that put the mother or baby at increased risk, or in the case of multiple births. Other than a higher incidence of multiple births, ART does not increase the risk to the fetus.
The miscarriage rate is about the same for ART as the general population. Many times older females undergo ART and their miscarriage rates are naturally higher. Since pregnancy testing is done two weeks after embryo transfer, we often know about spontaneous miscarriages in the very early stages of pregnancy. These miscarriages would probably go unnoticed in the general population.
Sperm quality on the day of egg retrieval is often related to what happened in the male’s body 3 months ago. This is because sperm development takes 3 months. Listed below are guidelines to help ensure the semen specimen is of the best possible quality.
- A fever of 101 degrees Fahrenheit or higher within 3 months prior to ART treatment may adversely affect sperm quality. Sperm count and motility may appear normal, but fertilization may not occur. If you become sick during the ART cycle, please notify the ART nurse, and take Tylenol to keep your temperature below 101 degrees Fahrenheit.
- Discontinue alcohol and cigarette use before and during ART treatment. Do not use any “recreational”/illegal drugs.
- If any prescription medication has been taken during the last 3 months, notify the ART nurse.
- Do not sit in hot tubs, spas, Jacuzzis, or saunas during or 3 months prior to the ART cycle.
- Do not begin any new form of endurance exercise during or 3 months prior to the ART cycle. Physical activity at a moderate level is acceptable and encouraged.
- Avoid all testosterone, DHEA, and Androstenedione/Androstanediol hormone containing supplements. NO GYM SUPPLEMENTS!
- Tell your infertility physician if you have ever had genital herpes, or suspect you may have been exposed to genital herpes in the past. Also tell your physician if you have pre lesion symptoms, develop a lesion, or have healing lesions before or during the ART cycle.
- Refrain from ejaculation for 2-3 days, but not more than 5 prior to collecting the semen sample for the ART cycle. The ART nurse will have your specific instructions from the Andrologist.
Your physician will discuss this with you at the time of consent signing, but we usually follow the recommendations of The American Society for Reproductive Medicine guidelines:
- Under 34 years old = 1-2 embryos
- 35-37 years of age = 2-3 embryos
- 38-40 years of age = 3 embryos
These numbers may vary depending on individual diagnosis and clinical circumstance.
A woman is born with a full complement of eggs. There are far more eggs than will ever be used during a normal lifetime and ART procedures have no measurable “lowering” effects.